4 min read
How to Save Billions Annually in Health Care
Cassie Schmalzl : 9.20.19 9:20 AM
It’s not news to state that health care costs are increasing to unprecedented levels, far above the growth rate of comparable countries. But beyond the obvious expenses of care, there are additional inconspicuous costs in our industry. Less noticeable costs – such as administrative tasks for health systems and payers alike – impact spending far more than may be realized.
A new report from Humana and the University of Pittsburgh quantified the wasted annual costs in health care. According to their research, between $760 billion and $935 billion—or about a quarter of all U.S. healthcare spending—is spent on waste. The analysis estimates most waste stems from $265.6 billion in administrative complexity.
One of the quickest, most successful paths to decrease costs is to reduce printing.

Print By Numbers
The average 1,500 bed hospital prints more than 8 million pages per month—96 million pages annually—adding up to $3.8 million dollars per hospital, per year. This is just the cost of paper and ink and doesn’t even account for the printing devices. The total annual cost to US physician practices for interacting with health plans is estimated at $31 billion dollars, which breaks down to $68,274 per physician, per practice.
Another staggering statistic: 60% of a hospital’s print volume—over 57 million pages annually–originates from their EHR, systems designed to eliminate the burden and risks of paper-based health care.
In this blog post we will focus on one category of EHR originated printing: sending and receiving attachments.
Why Attachments Cost So Much
An attachment is sent from a billing office to a health plan to provide additional clinical information about the patient’s care to inform reimbursement. In most cases, the attachment is sent when the billing office receives a denial. In other cases, attachments are sent with claims or used to obtain prior authorization. In value-based contracts, attachments may also be used for quality measures.
Attachments are costly for both sides, health systems and payers. “A regional health plan participating in the CAQH CORE Attachments Environmental Scan indicated that it takes 792 labor hours, the equivalent of nearly 20 people working full-time, to process the attachments it receives by mail, fax and web portal in the course of just one week.”
Health systems face similar direct costs in the staff required to print and mail or fax attachments (often referred to as ‘release of information’). However, these direct costs aren’t the biggest headache for health systems; the manual back-and-forth also increases accounts receivable (AR) days, the time it takes for the health system to be reimbursed for the care they’ve delivered. Finding a chart, reviewing for any release restrictions, printing, faxing and then mailing is a time consuming process that can have a meaningful impact on cash flow and operations. Thankfully, there’s a solution. The CAQH survey estimated that “adoption of electronic attachment transactions could reduce healthcare industry per-transaction costs for exchange of attachments by over 60%.”
A current electronic option that most payers have recently offered is web portals for health systems to upload attachments, as an alternative to printing and mailing. Adoption of the portals is minimal, because it requires additional effort beyond the current workflow and it doesn’t reduce the manual intensiveness required. Each chart still needs to be manually reviewed, saved, and uploaded individually to the payer portal, a website specific to each payer.
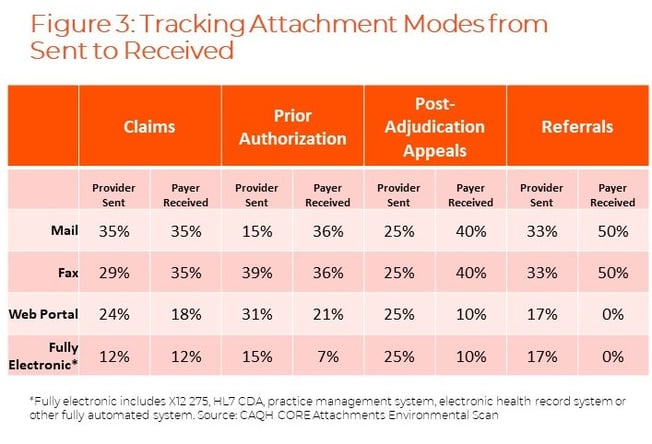
The following chart outlines the transmission modes for each attachment use-case. Indicating that over 50% for each use-case still relies on manual, paper-based workflows of mail and fax.
Security Risks of Analog Attachments
What’s worse, manual sending of attachments isn’t only more expensive, it’s also less secure. The top 3 ways printing sensitive patient data compromises security are:
- Leaving documents on the printer: Leaving documents containing sensitive information on the printer creates the risk that anyone—a visitor, non-administrative professional or health care provider not on the patient’s care team—could pick up the papers
- Storing patient data on printer hard drives: Many printers contain a hard drive which stores recent print jobs, posing an opportunity for hackers to identify an unlikely target containing patient data for ransom
- Relying on employee training for security compliance: Printing puts organizations in a position to rely solely on policies and employee training to enforce security, leaving an opportunity for human-error
Why Healthcare is Slow to Automate
In an age distinguished by digitization, these statistics are befuddling. How could this be? Why are health systems and payers spending so much on manual, outdated workflows?
One reason is data variability.
The industry has recognized the problem and has created calls to action. Legislation has provided an incentive. HIPAA, passed in 1996, established a mandate for all HIPAA covered entities to adopt fully electronic administrative transactions. The Affordable Care Act (2010), expanded on these mandates. More recently, CMS is pilot testing a proactive compliance review, which could impose penalties on HIPAA covered entities found non-compliant with federal mandates.
There are challenges. The size and metadata of attachments will vary from patient to patient. Historically, manual intervention has been required for billing offices to identify the right content to send in an attachment. And coders and trained specialists remain an essential step in interpreting patient charts. Additionally, variations in the content payers expect has been a barrier to automation.
But access to consistent, raw data would resolve a number of these issues.
How to Save Billions in Healthcare
A solution will require the industry to work together. There are a few potential options for success:
- Universal adoption of a structured attachment format: such as X12 277, X12 275 and HL7 CDA and standard documentation requirements across payers
- Incorporate natural language processing: an artificial intelligence technology, into reviewing attachment content can reduce the manual effort needed
- Utilize a clinical data partner: partner with an API platform, like Moxe’s. Our solution allows you to process all required information within your current EHR workflow, no printing or portals required. Since the platform is digital, secure, and automated, you’re able to process requests in a fraction of the time. This allows your staff to focus on higher complexity tasks while Moxe automates the majority of requests for clinical data
Connect with Moxe to see how you can reduce your print budget by more than 60%.